|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Society for the Advancement of Transplant Anesthesia

By Sergio
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
By Sergio
By Flora Simmons, MD
UNOS Launches National Liver Pairing Program
In an effort to increase access to living donations, UNOS has initiated a national pairing program for swapping livers. While some transplant centers have swapped livers within their own hospitals, this program now allows swapping across the nation.
Waiting Time Adjustment Approved For Kidney Transplant Candidates Affected By Race-based Calculation
After discontinuing race-based calculations for estimated glomerular filtration rate (eGFR), the new policy will now allow African-American kidney transplant candidates to receive waiting time modifications that will increase their waiting times and associated prioritization for transplant.
National Collaboration To Increase DCD Lung Transplantation Underway
UNOS recently launched a national initiative to identify and share effective practices that can increase transplantation of DCD lungs. Twenty-nine lung transplant programs are participating in this project.
By Michael Trostler, MD
LTRS is a useful predictor of Mortality that has been validated in the United States, but not in Europe. Based on the data the European registry collects, the score has been modified to exclude Diabetes. Age, BMI, MELD score, and Dialysis status were used with linear correlation for 90-day and 1-year mortality for each point. Included 2nd article external validation of LTRS in US (2020).
Validation of the Liver Transplant Risk Score in Europe.pdf
Preoperative Stratification of Liver Transplant Recipients- Validation of LTRS.pdf
Case report of a 54 year old Female who had a prolonged living donor liver transplant (1037 min) and massive blood loss (22.5L) who was successfully managed with Remimazolam without recall or adverse events with EEG monitoring.
Anesthesia Management of a Liver Transplant Recipient with Remimazolam.pdf
Large epidemiological study on 119,275 Liver transplant patients, with 2,820 living donor transplants which found a 13-17 year life gain for those who received a liver donor transplant for MELD>11, compared to those who stayed on the waiting list. This article generated significant interest with several comments/letters and the original authors reply which are well worth your time to read.
Survival Benefit of Living Donor Liver Transplant.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 1.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 2.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 3.pdf.
An updated review article of end stage liver disease scoring systems and their inherent weaknesses. The future may be artificial intelligence, but its predictive algorithms can be individualized and may not be applicable to the wider population outside of each study cohort.
A concerted push via QA/QI project achieves safety and success for immediate extubation of liver transplant recipients in both low risk and high risk patients. There was no change in mortality and only four(1.26%) patients were reintubated within 24 hours (Total 317 patients). Quality initiative pushes immediate extubations from 13.4% to 86.7% over a five year period.
By Alex Stoker, MD
IVC stenosis during liver transplant detected with TEE
Acute inferior vena cava (IVC) stenosis after liver transplantation is a rare but significant complication that can result in liver allograft congestion and dysfunction as well as hemodynamic instability. Transesophageal echocardiography (TEE) may be used to diagnose IVC stenosis, which may reveal a high velocity or turbulent jet entering the right atrium from the IVC as detected with color flow Doppler (CFD) (see figure below). By interrogating the IVC, it may be possible to visualize the area of narrowing within the IVC, with CFD revealing flow acceleration and turbulent flow originating at the level of stenosis. Obstruction may occur in the suprahepatic IVC, infrahepatic IVC or hepatic veins and can be due to surgical complication or due to thrombosis. There is increasing use of TEE to evaluate hepatic and IVC vasculature during liver transplantation (Khurmi et al, 2019). Reference
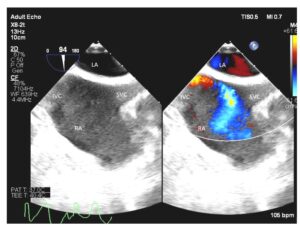 Midesophageal bicaval view with color compare showing the image both with and without color flow Doppler. A turbulent and high velocity jet is seen entering the right atrium from the IVC due to IVC stenosis. LA, left atrium; RA, right atrium; IVC, inferior vena cava; SVC, superior vena cava.
Midesophageal bicaval view with color compare showing the image both with and without color flow Doppler. A turbulent and high velocity jet is seen entering the right atrium from the IVC due to IVC stenosis. LA, left atrium; RA, right atrium; IVC, inferior vena cava; SVC, superior vena cava.
By Alexandra Ruan, MD
https://unos.org/news/2022-organ-transplants-again-set-annual-records/
By David Rosenfeld, MD, FASA
For this winter’s section we reached out to Spencer Liebman, MD, who is Chief, Division of Transplant Anesthesiology at VCU. Formerly known as Medical College of Virginia, VCU is an 820 bed health system and one of the nation’s first transplant programs. This historic program is named for David M. Hume, MD and Hyung Mo Lee, MD, and is where one of the earliest identical twin kidney transplants was performed in 1957, with the overall program starting in 1962. Soon after livers began in 1964, with the world’s 16th heart transplant in 1968. The scope of organs includes livers, kidneys, pancreas, and hearts, with experience in combined heart-liver transplant. A total of 502 organs were transplanted in 2022.
VCU offers 112 ICU beds, 16 of which are cardiac, and a dedicated transplant ICU growing to 10 beds under the direction of Megan Rashid, MD. The liver practice is large with 168 total adult organs, 21 of which were from living donors. Staffing is in a team care model with five dedicated attendings, six specially trained CRNAs, and residents rotating in their CA2/CA3 years. TEG is universal, and TEE is utilized for greater than 80% of cases. As is becoming more common, intraoperative hemodialysis (not CRRT) was used in 40% of cases in 2022. They offer a unique Active Severe Alcoholic Hepatitis Transplant Program with support services and strategies in place. VCU has a non-ACGME liver fellowship with a hybrid model of combined fellow and faculty time and two positions per year. In 2016 the Total Pancreatectomy with Islet Cell Autotransplant (TPIAT) program was started with the addition of Transplant Surgeon Marlon Levy, MD to the faculty. A total of 18 TPIATs were performed in 2022 for chronic pancreatitis, and they are one of the few centers offering this experimental therapy. Their cardiac program is the longest running on the east coast and the second oldest in the US. Over 680 heart transplants have been performed, and they offer an ACGME accredited Adult Cardiothoracic Anesthesiology fellowship with two fellows per year. There are no lung transplants being performed at present.
Many thanks to Dr. Liebman for sharing details of the transplantation program at VCU. If interested in having your program highlighted in the future, please contact David Rosenfeld, Mayo Clinic Arizona at Rosenfeld.david@mayo.edu
*The original newsletter identified VCU as performing the first identical twin kidney transplant in 1957. This was in error, the first kidney transplant was performed in an identical twin by Dr Joseph E.Murray in Boston in 1954. Correction made above.
By Susan Mandell, MD
We look forward to seeing SATA members at the in person SATA National Meeting, held at the IARS on April 17th, 2023, in Denver Colorado. Please remember to renew your membership for free entry to the meeting. SATA is pleased to announce it will hold the first combined meeting with the International Liver Transplant Society-SATA meeting just prior to the ASA in San Francisco. This has been a very popular meeting and well attended.
The Council is pleased to announce that there are now seven regional SATA meetings. Please check for the meeting closest to you. Service on the SATA Accessibility and Diversity Committee is now open to all members. The Vanguard committee has been revitalized and membership is open to all faculty who are within 5 years of residency completion or are younger than 42, please reach out to the SATA Office for more information.
We are pleased to announce that SATA will be represented at the 10th Annual Korean Society of Transplant Anesthesiologists (KSTA) meeting in Seoul, Korea. During the Joint KSTA-SATA session (March 18, 2023 11:20-12:50 KST), moderated by Dr. Tetsuro Sakai and Justin Sangwook Ko, Dr. Satish Kumar will present on emerging evidence for coronary artery disease screening in liver transplant candidates and Dr. Ramona Nicolau-Raducu will present on post-reperfusion hyperfibrinolysis.
SATA is delighted to endorse the first International Symposium for Abdominal Organ Transplant (ISAOT) in Santiago, Chile, June 8-9, 2023.
This opportunity is presented by Dr. Klaus Torp at Mayo Clinic-Jacksonville (Founding member of SATA) who has supported the physician exchange program with the Clinica Alemanha in Santiago de Chile. Dr. Lucile Gignon (Faculty Anesthesiologist at the Clinica Alemanha in Santiago de Chile) is the local organizer of the meeting.
Attention liver transplant anesthesiologists and program directors! SATA is offering free 6 month membership to fellows! Please sign up by emailing sata@pacainc.com. We look forward to welcoming new fellow members!
Join the Vanguard Committee ***
SATA Meetings
SATA Tristate Regional Meeting – in person and virtual
March 25th, 2023, New York, NY
April 17th, 2023, Denver, CO
Other Meetings:
The 10th annual scientific meeting of the Korean Society of Transplantation Anesthesiologists (KSTA), March 18th, Seoul, Korea – in person and hybrid
Joint KSTA-SATA Session: 11:20 – 12:50 KST
IARS/AUA/SOCCA Annual Meeting – in person and hybrid
April 13-16th, 2023, Denver, CO
The 2023 International Congress of ILTS, ELITA and LICAGE
May 3-6, 2023; Rotterdam, Netherlands
American Transplant Congress (ATC) 2023 Annual Meeting
June 3-7, 2023, San Diego, CA
International Symposium for Abdominal Organ Transplant (ISAOT)
June 8-9, 2023, Santiago, Chile
By Sergio
|
Michael Trostler, MD
Highlights: South Korean study of 398 patients evaluating incidence of post-reperfusion syndrome in a propofol vs sevoflurane anesthetic, found a statistically significant decrease in the sevoflurane group.
2. Outcomes of Bariatric Surgery Before, During, and After Solid Organ Transplantation
Highlights: Bariatric surgery was able to be performed safely, pre-transplant, simultaneously with transplant, or post-transplant with no increase in adverse events related to the bariatric procedure. Bariatric surgery leads to weight loss and decreased comorbidities in this patient population.
3. Orthotopic Transplantation of the Full-length Porcine Intestine After Normothermic Machine Perfusion
Highlights: The new trend of machine perfusion in organ transplantation is at the forefront of transplantation and extended criteria organs. Porcine model of intestinal transplant has been shown to be viable and successful.
Highlights: A review article of 9 studies including 2000 patients shows no increase in disease free survival, HCC recurrence or impaired overall survival. If cell salvage is desired, it should not be immediately disregarded as an option just because of a hepatocellular carcinoma diagnosis.
Highlights: After a peak in living donor liver transplants in 2001 there was a fall, but there has been a steady rise from 2011 to 2019. There have been improvements in transplant survival over the years with a significantly decreased mortality over the past few years compared to the first few years.
|
|
For this quarter’s segment, we connected with Dr. Govind Rangrass, MD, Director of Transplant Anesthesia and Director of Quality/Patient Safety at the new 400-bed SSM Health/Saint Louis University Hospital (SLUH).
Saint Louis University has a long history with abdominal transplant, at one time being one of the busiest transplant centers in the country. In recent years, their volumes have hovered between 30-40 liver transplants/year. SLUH recently merged with the SSM Health, a large hospital network, and as its only transplant center, the program is gearing up for an increase in transplant evaluations and referrals and is carefully navigating the listing process for high-risk patients.
As part of the selection process, the transplant anesthesia director sits on the Liver Recipient Selection Committee. A unique aspect of their program is that they have a separate High Risk Cardiac Evaluation Meeting, which meets weekly to discuss candidates with complex cardiac disease who may benefit from additional pre transplant work-up optimization and ensure postoperative continuity of care with the cardiology team. One of their transplant faculty was the corresponding author of the newly released AHA Scientific Statement on Coronary Heart Disease Screening in Kidney and Liver Transplantation Candidates published in Circulation. Between 2019-2021, patients undergoing liver transplantation at SSM Health/SLUH had 100% survival at one month and 94% survival at one year post transplant.
Their program is one of the few that uses alternative portal flow in transplant for patients with portal vein thrombosis using reno-portal (connecting left renal vein of recipient to donor portal vein to act as inflow) and gastro-portal (using left gastric vein as inflow) anastomoses. Another unique aspect of the program is the disproportionately high number of hepatitis C positive donor livers utilized (~20%). Their program is gaining more experience with the Transmedic normothermic perfusion pumps, which it intends to continue using in the future.
TEG 6S is routinely used and available and housed in the hospital coagulation lab, with a real time tracing available in the operating room. Venovenous bypass is used selectively for redo liver transplants, patients with portopulmonary hypertension with RV dysfunction or hepatopulmonary syndrome, and high MELD patients on preoperative CRRT. Heparin (50U/kg) is administered for hypercoagulable patients prior to caval cross-clamping, and antifibrinolytics are administered as a bolus during the anhepatic stage. Octreotide infusions (50mcg bolus followed by 100mcg/hr) are routinely run for patients with significant portal hypertension.
The SSM Health/SLUH transplant program hosts a robust outcomes research center and has multiple grant-funded research projects. Examples include a study on biomarkers of kidney function to predict perioperative acute kidney injury; a normothermic perfusion basic science lab studying pharmacologic tools to reduce ischemia reperfusion injury in discarded human livers placed on perfusion pumps; and a $1.8 million grant in conjunction with Missouri University of Science and Technology to develop artificial intelligence driven decision-making tools for organ allocation.
Announcements
The Accessibility and Inclusion Committee
The SATA Council is pleased to announce the introduction of The Accessibility and Inclusion Committee. The Committee will help develop SATA policies by providing the Council with their views on how to ensure members have equal access to all service opportunities within the organization, All SATA members are invited to nominate themselves or a colleague to serve on this new important committee as part of the society leadership. Please send your nominations to the SATA Secretary: Lorenzo De Marchi at demarchilorenzo@yahoo.com
Service: Appointment by SATA Council
Term: 2 years; can be renewed
Requirements: SATA Membership in good standing
Purpose: Oversight and Advocacy Committee
Seed Grant Funding Mechanism
The SATA Seed Grant is a one-year $5,000 transplant project starter grant, open to junior faculty members and trainee physician members of the Society. The grant aims to inspire and assist aspiring faculty/trainee physicians who have yet to receive any previous funding to start a transplant-related project. The grant requires the recipient to submit a support letter from the mentoring faculty and the Department Chairperson.
Application/Grant Cycle:
November 1, 2022 – Announcement of the grant
December 1, 2022 – Opening of the submission site
February 28, 2023 – Closure of submission site
April 1, 2023 – Announcement of the awardee and send letters of feedback to the other applicants
April 17, 2023 – Grant presentation at SATA National Meeting in Denver, CO
July 1, 2023 – Grant initiation
December 31, 2023 – submission of the mid-term report
June 30, 2023 – submission of the final report
Click here to review the SATA Seed Grant Grading
Click here to review the SATA Seed Grant Proposal
SATA Meetings
Southeastern SATA Regional Meeting: November 5, 2022
SATA West Meeting: December 10, 2022, San Francisco – in person and hybrid.
Submit an Abstract by email to: Dieter.Adelmann@ucsf.edu
Mid-Western SATA Regional Meeting: January 21, 2023
Other Meetings:
The Liver Meeting – aasld.org, November 4-8, 2022, Washington, DC
The 2023 International Congress of ILTS, ELITA and LICAGE
May 3-6, 2023; Rotterdam, Netherlands
American Transplant Congress (ATC) 2023 Annual Meeting
June 3-7, 2023, San Diego, CA
By Sergio
By Flora Simmons, MD
OPTN Board Eliminates Race-based Calculation For Transplant Listing
In a momentous measure to provide equitable access to all transplant candidates, the board of directors of the Organ Procurement and Transplantation Network recently approved a precedent requiring transplant hospitals to use race neutral calculations when estimating a candidate’s glomerular filtration rate (GFR). Read more here.
Kidney Transplants have Increased in Minorities since Policy Changes
Following implementation of the updated allocation system, one year monitoring reports show that transplant rates increased significantly for several key populations including Black, Hispanic, Asian, and pediatric candidates. The updated allocation system replaced the donation service area and administrative regions with a 250 nautical mile circle around the donor hospital. Read more here.
By Michael Trostler, MD
“Abdominal Organ Transplantation: Noteworthy Literature in 2021”– Seminars in Cardiothoracic and Vascular Anesthesia
Highlights: Yearly article by corresponding author, SATA president Dr. Tetsuro Sakai, selecting 20 articles from over 10,000 articles published over the year. Read the article here
“Analysis of outcomes and renal recovery after adult living-donor liver transplantation among recipients with hepatorenal syndrome” – American Journal of Transplantation
Highlights: Retrospective analysis of 2185 living donor liver transplants over a 7 year period found that time from HRS to transplant was significantly associated with recovery, and recovery was significantly associated with survival. Read the article here
“Hypothermic oxygenated perfusion in extended criteria donor liver transplantation—A randomized clinical trial” – American Journal of Transplantation
Highlights: Machine perfusion is at the forefront of new technological innovation in the transplant community. A randomized control trial of HOPE in 110 extended criteria donors found improved outcomes with lower graft dysfunction and better graft survival. Read the article here
“Transplantation of a human liver following 3 days of ex situ normothermic preservation” – Nature Biotechnology
Highlights: 3 days of Ex-Vivo machine perfusion prior to transplant was successful and at one year follow-up the recipient was alive and the biliary tree intact. Read the article for the amazing details here
“Final Safety and Efficacy Results from a 106 Real-World Patients Registry with an Ascites-Mobilizing Pump” – Liver International
Highlights: 12 European centers have followed 106 patients over 24 months with a “Alfapump”, an intraperitoneal fluid management system that pumps ascites from the peritoneal cavity into the bladder for excretion. Designed for those ineligible for a TIPS procedure. Read the article here
“Sequential liver and kidney living donors: Making the ultimate gift twice” – Clinical Transplantation
Highlights: 150 living donors in the United States have donated more than one organ. 20 of these donors donated at UPMC- Pittsburgh, with 70% non-directed/altruistic with first donation and 80% non-directed/altruistic at the second donation. Read the article here
By Alex Stoker, MD
Imminent Death Donation
Imminent death donation (IDD) is a proposed organ donation practice described as the recovery of a living donor organ immediately prior to an impending and planned withdrawal of ventilator support expected to result in the patient’s death [OPTN white paper, 2016]. This practice is aimed at increasing the availability of donated organs through increased utilization of organs from donors who may have had non-progression during attempted DCD donation and by reducing organ ischemia. In 2016 the ethics committee of the Organ Procurement & Transplantation Network (OPTN) outlined several ethical concerns, potential risks, as well as challenges of IDD; however, acknowledged the possibility of overcoming those challenges in the future [OPTN white paper, 2016]. A recent survey by Washburn et al explored the public attitudes towards IDD in the United States and describe a scenario in which one kidney, a portion of liver and portion of lung are donated prior to withdrawal of life support [Washburn et al, 2020].
Read more from reference here
Rise of the Machines – Normothermic Ex Vivo Perfusion in Liver Transplantation
Since the first use of normothermic machine perfusion (NMP) in human orthotopic liver transplantation in 2013 there has been considerable and growing interest in using NMP to improve organ quality prior to transplantation by maintaining the allograft in a physiologic state during transportation. While ongoing investigations have yet to confirm all the potential benefits, NMP may reduce allograft ischemic damage, lessen the metabolic and hemodynamic derangements following liver reperfusion, increase the utilization of marginal organs, improve transplant logistics and expand the donor pool.
Read more from reference here
By David Rosenfeld, MD; Alex Stoker, MD
For this summer’s piece we choose to focus exclusively on the adult cardiac and lung transplant program at Duke. A large medical center with 1048 patient care beds, Duke University Hospital is one of the premier centers in the world for cardiac and lung transplantation. According to 2021 SRTR data they were third in the US in adult cardiac transplant volume with 104, second in lung with 108, and also performing three combined cardiac-lung transplants, and one lung-liver transplant.
Led by Dr. Mihai Podgoreanu, the Duke Cardiothoracic Anesthesiology Division has been a leader in comprehensive perioperative management of thoracic organ and combined organ transplant recipients as members of the Duke Transplant Center, which recently celebrated its 10,000th transplant milestone. Perioperative transplant care is provided by a highly integrated group of cardiothoracic anesthesiologists and intensivists, 4 or 5 anesthesia residents, and up to 10 fellows covering a total of 9 adult cardiothoracic operating rooms and 32 CTICU beds. Duke has one of the largest and busiest Adult Cardiothoracic Anesthesia (ACTA) fellowship programs in the US (14 fellows/year), led by Dr. Brandi Bottiger who also directs Quality Improvement across the Duke Transplant Center. Concomitantly, the Anesthesiology Critical Care Medicine (CCM) fellowship program, led by Dr. Nazish Hashmi, is rapidly growing (8 fellows/year), with a strong emphasis placed on acute care of critically ill transplant patients. Thoracic transplant recipients recover in the cardiothoracic intensive care unit (ICU), which offers 24/7 coverage by anesthesiologists with cardiothoracic and critical care training. The ACTA and CCM fellows participate in multidisciplinary care of these patients along the continuum from the operating room and through the cardiothoracic ICU, while gaining an unparalleled experience in perioperative echocardiography, complex cardiopulmonary and mechanical circulatory support physiology.
The Duke Heart Transplant program, under the medical directorship of Dr. Adam Devore, has a comprehensive patient selection process where many disciplines are represented, including anesthesiologists and intensivists. Performing the first donation after circulatory death (DCD) case in 2019, the cardiac transplantation program has completed more than 80 heart transplant procedures with DCD donors. To facilitate this innovative practice which significantly expands the donation pool, Duke has been early in its use of the Transmedics Organ Care System (OCS) and is one of five centers included in a prospective non-inferiority trial comparing transplantation of DCD organs resuscitated with the device compared to donation after brain death hearts preserved with traditional cold storage methods. Dr. Jacob Schroder is the surgical director of heart transplantation and the principal investigator for the OCS DCD heart trial, which helped support the FDA’s approval of the device for DCD donor hearts in April 2022.
Similarly, the Duke Lung Transplant program, under the medical directorship of Dr. John Reynolds, has a comprehensive, multidisciplinary patient selection process. Anesthesiologists are involved in developing quality metrics and improvements in clinical care. The Duke Lung Transplant program, with surgical director Dr. John Haney, has adopted elective intraoperative VA ECMO during lung transplantation to reduce allograft reperfusion injury, increase cardiopulmonary stability, and reduce comorbidity associated with cardiopulmonary bypass use. They utilize a hybrid ECMO circuit that can be quickly converted to a full CPB circuit if needed emergently.
Transplantation is truly a team sport at Duke, with a dedicated multidisciplinary team in place to care for these complex patients.
Many thanks to Dr. Bottiger for sharing details of the transplantation program at Duke University Medical Center. If interested in having your program highlighted in the future, please contact David Rosenfeld, Mayo Clinic Arizona at Rosenfeld.david@mayo.edu
Attention liver transplant anesthesiologists and program directors! SATA will be offering free 6 month membership to fellows! Please sign up by emailing sata@pacainc.com. We look forward to welcoming new fellow members!
SATA Meetings:
Midstate SATA Regional Meeting: September 24, 2022
Southern SATA regional Meeting: November 5, 2022
Mid-Western SATA Regional Meeting: January 21, 2023
Other Meetings:
ILTS Perioperative Care in Liver Transplantation Meeting 2022
October 21, 2022; Ochsner Health, LA; in-person and virtual
The 2023 International Congress of ILTS, ELITA and LICAGE
May 3-6, 2023; Rotterdam, Netherlands
American Transplant Congress (ATC) 2023 Annual Meeting
June 3-7, 2023, San Diego, CA
By Sergio
By Flora Simmons, MD
Liver transplant rates increase after implementation of new organ allocation policy
The OPTN data report is now available and describes key measures of the new liver and intestinal allocation policy for the 18-month period from February 2020 through August 2021. Results show an overall increase in deceased donor liver-alone and liver-kidney transplants, significantly increased transplant rate for sicker patients, and more transplants being performed between 250 and 500 nautical miles, leading to slightly longer median cold ischemic times. Read more here.
Record setting year for heart, liver, and kidney transplants in 2021
For the first time, organ transplants in the United States exceeded 40,000 for a grand total of 41,354 organs transplanted in 2021. There were a total of 24,669 kidney transplants, 9,236 liver transplants, and 3,817 heart transplants. Heart transplants have set a new record for the past 10 consecutive years, while liver transplants have set annual records for the past nine years. Read more here.
DCD Procurement Collaborative Project surpassed goal and recovered DCD donors at a higher rate than the rest of the nation
Twenty-six OPOs from across the country collaborated with the aim to increase the number of DCD donor procurements. Improvement efforts were focused across multiple areas including strengthening relationships between donor hospitals and transplant programs and optimizing clinical practices. The cohort procured 34% more DCD donors in 2021 compared to 26% for the rest of the nation. Read more here.
From Susan Mandell, MD and David Corey, MBA
SATA is excited to announce a new partnership with Corey & Associates (PACA) that will assist with the day-to-day business management of the society’s activities. PACA has worked in the area of management and government relations since 1975, SATA looks forward to working with PACA in order to improve this membership experience. Please find a link to PACA on our webpage here
By Yong G. Peng, MD, PhD, FASE, FASA
With the help of SATA treasurer Dr. Jiapeng Huang preliminary communication, SATA executive council members Drs. Tetsuro Sakai, Jiapeng Huang and Susan Mandell had a Zoom meeting with the Society of Cardiovascular Anesthesiologists (SCA) leadership group. This was a productive discussion covering a wide range of potential collaborations between SCA and SATA.
SCA’s president Dr. Andrew Shaw has fully endorsed Drs. Archer Martin of Mayo Clinic Jacksonville and Sharon McCartney of Duke to become the inaugural Co-Chairs for the Transplant Anesthesia Subcommittee of SCA. Together they will oversee all the projects and progress of collaboration between SATA and SCA.
The initial area of mutual interest will include the following:
In response to the call for SATA and SCA collaborations, both SATA’s CT Transplantation Committee and CT Educational Task Force Committee recently had a Zoom meeting to lay out the specific action plans. The committees proposed that SATA has three cardiothoracic related entities (CT transplantation Committee, TEE Work Group and CT Educational Taskforce) working together to consolidate resources and make a collective effort to reach important goals. These include promoting cardiothoracic related missions of SATA to other societies scientific activities, distribution of cardiothoracic transplantation educational materials on the SATA website, hosting regular meetings on relevant cardiothoracic transplant topics to maintain SATA member’s interest, and keeping all three entities member engagement to advance SATA’s clinical and research interest in collaboration with other professional societies.
By Michael Trostler, MD
Highlights: Hypothermic machine perfusion decreases post-reperfusion syndrome and early graft dysfunction. Normothermic machine perfusion reduces incidence of post-reperfusion syndrome and early graft dysfunction. Normothermic regional perfusion decreases likelihood of early graft dysfunction and risk of primary non-function. Read more here
transplantation of high-risk donor livers
Highlights: Sequential Dual hypothermic oxygenated machine perfusion followed by Normothermic Machine Perfusion (DHOPE-NMP) was used to salvage 63% of originally discarded livers with 1 year graft survival 94%, and patient survival 100%. Read more here
Highlights: Mortality after liver resection is nearly 50% higher than liver transplant in hepatocellular carcinoma. Read more here
By Michael Ander, MD
Highlights: Donor age, donor BMI, moderate macrosteatosis, and CIT were identified as risk factors for the development of PRS in LT using DBD grafts. PRS risk evaluation may improve donor-to-recipient matching based on their MELD scores. Read more here
Highlights: Results provide evidence that overweight and obesity class 1 are associated with decreased length of stay and mortality following liver transplant, while underweight and obesity class 3 are associated with prolonged length of stay. Read more here
By David Rosenfeld, MD, FASA
For this quarter’s segment we were able to connect with Scott Lindberg, MD, FASA, director of liver transplant anesthesiology at the 900 bed Houston Methodist Medical Center.
Currently Methodist is one of the busiest abdominal programs in the US with 183 livers, 255 kidneys (47% live donor), and 14 pancreas cases completed in 2021. For the liver program nearly all are cadaveric, however they have launched a liver donor program with their first case in October 2021, and a second scheduled in early 2022. Methodist is aggressive in utilizing advanced age/extended criteria grafts with over 20% DCD. They are frequently using the Transmedic normothermic perfusion system and are working to publish their early experience. Nearly all cases are on VV bypass, PA catheter and FloTrac are routine, TEE is placed in nearly 100% of cases with one team member advanced certified. ABG assays are POC in-room. ROTEM is performed in the central lab; however, the tracing is visible in real time in the OR. Antifibrinolytics are given with documented hyperfibrinolysis in conjunction with on field coagulopathy, and in cases when greater than eight units of packed cells are administered. A small percentage of patients are extubated in the operating room.
The most unique aspect of the liver transplant anesthesiology practice is that it is covered exclusively with a dedicated six-physician team from the private practice group US Anesthesia Partners working either as the sole in-room provider or in conjunction with UT Houston anesthesia residents, who rotate late in the CA2 and throughout the CA3 years. Team members carry faculty appointments at the Weill Cornell School of Medicine and/or Texas A&M College of Medicine. This private staffing model is clearly uncommon, and particularly unusual given that the program was the third largest volume US center in 2021. Several years ago, Methodist hired liver transplant anesthesiologist Randolph Steadman, MD, MS, to serve as Chair of Anesthesiology, to lead the hospital-based group, and to increase collaboration between the private and hospital practices. In that vein, in September 2021 the department was accredited for an anesthesiology residency, with Dr. Lindberg of US Anesthesia Partners in the role of program director. It is an exciting time as they recently matched their first class of six categorical residents to begin in July 2022.
The transplant program has made it their mission to expand the donor pool by looking to technology and data to push the boundaries of extended criteria donors. There is also a commitment to increase research activity with the establishment of the residency program.
SATA Tristate Liver Anesthesiology Meeting, NYU School of Medicine, April 9th, 2022; 9:00 am – 2:00 pm EST. Click here to Register Click here to review the Program Agenda
SATA Virtual Lung Transplant Anesthesia Fellowship Series, April 16, 2022 6:00 PM EST. Dr. Jack Hanley will be interviewed by Dr. Brandi Bottiger exploring a surgeon’s perspective on lung transplantation. Click here for advanced registration. here
SATA East Regional Meeting, DMV Liver Transplant Anesthesia Meeting 2022. Virtual, April 23rd, 2022 8:45am – 12:45 pm EST. Click here for details here
ILTS Annual Meeting May 4 – 7, 2022, Istanbul, Turkey
American Transplant Congress June 4 – 8, 2022, Boston, MA
International Liver Transplant Congress June 22 – 26, 2022
ILTS Perioperative Care in Liver Transplant Meeting, October 21, 2022, New Orleans, LA
UTHealth Anesthesiology – Medical Co-Director of the Transplant Intensive Care Unit
The Department of Anesthesiology at McGovern Medical School at UTHealth is seeking applicants for the position of Medical Co-Director of the Transplant Intensive Care Unit (TSICU) at Memorial Hermann Hospital- Texas Medical Center.
The role of the Medical Co-Director is to oversee and integrate all clinical policies and practice standards in close cooperation and collaboration with the Chief of Transplant Surgery, Pulmonary Critical Care Medicine and other collaborating services in the Transplant Service Line. The Medical Co-Director will partner with the Chair of the Department and the Division Chief of Critical Care Medicine to promote a cohesive strategy to enhance patient care, structure educational systems, standardize translational research opportunities and infrastructure where appropriate and promote a culture of clinical excellence. Additionally, the Medical Co-Director will contribute to the transplant anesthesiology team and collaborate with hospital leadership including the Transplant Service line administrative and nursing teams.
Required qualifications:
If interested, please submit your CV and cover letter to:
George Williams, MD, FASA, FCCM, FCCP
Vice Chair for Critical Care Medicine, Department of Anesthesiology
McGovern Medical School at UTHealth
By Sergio
Flora Simmons, MD
David Rosenfeld, MD
An affiliation between Jackson Health System and UHealth-the University of Miami Health System.
In this month’s feature we learn from Drs. Ramona Nicolau-Raducu and Yehuda Raveh some of the characteristics that are unique about MTI.
The program is housed within the massive Jackson Memorial Hospital, one of the ten largest hospitals in the world with 2000 beds. Year in and out they are amongst the busiest abdominal programs with a US leading 472 kidneys transplanted in 2020, including a paired exchange program. MTI is also a front-runner in liver for the last 50 years, with over 4500 cases performed and 131 adult and 22 pediatric in 2020. Pancreas transplant is equally robust. For more than 20 years, and greater than 500 cases, a multidisciplinary team of experts at MTI has been treating thousands of children and adults with intestinal failure via Intestinal Rehabilitation or the Intestinal/Multivisceral Transplant Program, with outcomes well above national averages. Along with deceased donor intestinal (~5 cases/year) and multivisceral transplants (~10-15 cases/year), autologous transplant procedures are offered.
MTI became in recent years a bloodless center for Jehovah Witness transplants with a meticulous selection process for Jehovah’s Witness liver candidates. A bloodless protocol has been established of using factor concentrates, hemopure (bovine hemoglobin-based oxygen carrying solution) autotransfusion and cell saver.
In February 2020 the national organ allocation system transformed from donor service area-based to an acuity circles-based model. Due to its unique geography near the tip of the Florida peninsula, the new system limits organ allocation. As a result, use of DCD and other extended criteria grafts for liver or liver-kidney have increased, currently approximately 25% of liver grafts. In addition, patients listed for multivisceral transplantation are especially impacted by this change. Due to specific quality requirements for suitable donors, which are typically younger and non-obese, the available donor pool is considerably smaller. Previously these patients were assigned amongst the highest status levels on the liver match run, but the current allocation model routinely prioritizes a suitable donor to a liver alone candidate that does not have the same size and quality limitations but has a high “competitive” MELD score.
The Abdominal Transplant Anesthesia Fellowship at Jackson Memorial Hospital was created in 2006 by Dr. Ernesto Pretto, Chief, Division of Transplant Anesthesia and is one of the largest in the nation with 4 fellows/year. Transplant anesthesiology fellowships are non-ACGME accredited and are generally less popular for board eligible/certified US anesthesiology graduates, however this program has thrived through selecting highly qualified foreign graduates to consistently fill its positions. They have graduated a remarkable 50 transplant fellows in the last 15 years (10% US graduates and 90% International).
Many thanks to Drs. Nicolau-Raducu and Yahuda for sharing details of their program.
If interested in having your program highlighted, please contact David Rosenfeld, Mayo Clinic Arizona at Rosenfeld.david@mayo.edu
Michael Trostler, MD
Since 1996 Milan criteria for hepatocellular carcinoma has been used to guide liver transplantation to those who would benefit most and restrict deceased donor organs to those with the highest likelihood of survival. Living donor transplants tend to be directed to individuals who do not meet this criteria if the donor and recipient understand the potential risk. Liang et al. out of Taiwan report on 155 patients, 78 of which were beyond Milan criteria for tumor size or number found similar outcomes and recurrence rates. They propose a new criteria: maximum tumor size <= 6cm and total tumor size < 10cm.
There is potential to expand transplant criteria for living donor liver transplantation with less stringent criteria for directed donors. In addition to the potential for an expanded hepatocellular carcinoma guideline, cholangiocarcinoma is another disease process with historically poor outcomes which may be treated by transplantation with strict selection criteria, operative staging, and neoadjuvant therapy.
Ex-vivo machine perfusion – Meta-analysis included 34 articles with odds ratios favoring hypothermic machine perfusion over static cold storage. Findings include: decreased early graft dysfunction, ischemic cholangiopathy, non-anastamotic strictures and graft loss. Machine perfusion was associated with shorter length of stay. Normothermic perfusion is associated with reduced graft injury.
At the American Transplant Congress (June 2021) 33 abstracts on machine perfusion were presented including heart, lung, liver and kidney. Machine perfusion may become gold standard in the future as innovation and advancement bring down costs and improve outcomes.
Yong G Peng, MD, PhD
We caught up with the Quality and Standards Committee Chair, Dr. Adrian Hendrickse (Associate Professor, University of Colorado). The members of the committee have been working hard on several surveys. The first survey, led by Dr. Cara Crouch (Assistant Professor, University of Colorado), looked at Adult Liver Transplant Anesthesiology practice patterns across the US. Their research was published in the Journal of Clinical Transplantation. (Crouch et al. Clin Transplant. 2021)
Additionally, a smaller sub-committee of members are interested in living donor liver transplantation (LDLT) status. The group, headed by Dr. Tetsuro Sakai (SATA president), has investigated LDLT programs across the US. They have submitted their findings in an abstract to the 2022 IARS/AUA and ILTS meetings. They plan to prepare a manuscript of their findings. The committee has worked closely with the Korean Society of Anesthesiologists in an effort to write a collaborative review of LDLT practice, which they are planning to submit to Clinical Transplantation.
The Q&S committee members have worked on several other research projects, including similar survey-based methods, investigating different organ transplantation services, and pursuing the development of SATA endorsed guidelines for our subspecialty.
Lorenzo De Marchi, MD, Secretary, SATA
The SATA council wishes its members a happy holiday and new year. We are always looking for ways to ensure SATA meets your needs. Send us your suggestions. We are listening. Let us update you on the most recent and exciting projects in the works.
Membership renewal: We look forward to working with you in the upcoming year so don’t forget to renew for 2022. There is easy access on the website. New members will receive six months free SATA membership. Let your colleagues know.
The SATA-Data Collection Project; a collaborative data collection project that extends the American College of Surgeons NSQIP to anesthesia outcome measures of abdominal transplantation. Headed by Dieter Adelman an anesthesiologist from UCSF and Stuart Greenstein, a surgeon from Montefiore. If your center wants to participate, please reach out to Dr. Dieter Adelman (dieter.adelmann@ucsf.edu) and Dr. Sher-Lu Pai (pai.sherlu@mayo.edu) for information.
New Professional Associations: SATA and the Society for Cardiovascular Anesthesia have agreed to work together on shared interests in both heart and lung transplantation. We thank SATA President Dr. Ted Sakai and SATA Treasurer Dr. Jiapeng Huang, in addition to Dr. Archer Martin from SCA for their hard work on this project.
New Committee: SATA approves new Critical Care Medicine Committee. Please contact Dr. Ranjiit Deshpande through the SATA home link to apply and find out more.
Expanding SATA research: Go to the web to apply for the Society’s endorsement for your research project. Submit your application to the SATA Secretary (demarchilorenzo@yahoo.com) for Council review and feedback.
The SATA annual meeting at the IARS is in Hawaii on Monday, March 21th, 2022 as an in-person meeting. If you can’t be there don’t forget about upcoming SATA regional meetings with CME credits. Check on the Society’s website for a complete list and dates.
August 2021: Rise of the Machines in Solid Organ Transplant
February 2021: Pro/Con Debate: Routine Anticoagulation in Liver Transplantation
October 2020: Pro/Con Debate: ECMO vs Cardiopulmonary Bypass in Lung Transplantation
June 2020: Transplant Anesthesiology during the COVID-19 Pandemic
June 2021: Evaluation for Lung Transplantation: Pulmonologist Perspective
March 2021: Living Donor Liver Transplantation: Donor Management
August 2021: Cardiovascular Assessment of Liver Transplantation Candidates
June 2021: Multivisceral Transplantation
May 2021: Acute Liver Failure
SATA West Coast Liver Transplant Anesthesia Meeting, December 11, 2021 9am – 12:30pm PST – Register for the Virtual Meeting
SATA Midwest Meeting, January 22nd, 2022; 8:55 am – 12:30 PM CST – Register for the Virtual Meeting
SATA National Meeting at IARS, March 21, 2022, Honolulu, HI
SATA Tristate Meeting, April 9th, 2022
ILTS Virtual Consensus Conference January 28-29, 2022
IARS Annual Meeting March 18 – 21, 2022, Honolulu, HI
ILTS Annual Meeting May 4 – 7, 2022, Istanbul, Turkey
Are you enjoying the SATA Newsletter? Please fill out a quick survey!
President
Tetsuro Sakai, MD, PhD, MHA, FASA
Immediate Past President
M. Susan Mandell, MD, PhD
Founding President
Ernesto A. Pretto Jr., MD, MPH
President-elect
Gebhard Wagener, MD
Secretary
Lorenzo De Marchi, MD
Treasurer
Jiapeng Huang, MD, PhD, FASA, FASE
Executive Council
Ranjit Deshpande MBBS
Adrian Hendrickse, BM, PgDipMEd, MAcadMEd, FRCA
Christine Nguyen-Buckley, MD
Ramona Nicolau-Raducu, MD, PhD
Yong G Peng MD, PhD
Sennaraj Balasubramanian, MD
Amit Bardia, MD
Jiapeng Huang, MD, PhD, FASA, FASE
M. Susan Mandell, MD, PhD
Sergio Navarrete, DO
David Rosenfeld, MD
Flora Simmons, MD
Natalie Smith, MD
Michael Trostler MS, MD
By Sergio
New SATA Leadership Announced on August 1, 2021
Tetsuro Sakai, MD, PhD, MHA is the new President. The new SATA leaderships include Gebhard Wagener, MD (President-Elect: Columbia University), Lorenzo De Marchi, MD (Secretary: Georgetown University), and Jiapeng Huang, MD, PhD (Treasurer: University of Louisville), as well as Executive Councilors Ranjit Deshpande, MD (Yale University), Adrian Hendrickse, BM, FRCA (University of Colorado), Christine Nguyen-Buckley, MD (UCLA), and Ramona Nicolau-Raducu, MD, PhD (University of Miami). Dr. M. Susan Mandell serves as the Immediate Past President. Dr. Ernest Pretto, Jr. is the Founding President.
By Sergio
Flora Simmons and Susan Mandell
The SATA News teams would like to remind all SATA members of the upcoming elections for the executive council. Each member can cast a vote for two Councilor at Large and the Treasurer of the Society. Look for more announcements on this important upcoming election and cast your vote. Biographical snapshots of each candidate will be circulated to all SATA members to help you decide which candidate you want to help pave our path for the future.
Sathish Kumar and Yong Peng
On February 23rd SATA hosted a pro-con debate webinar on anticoagulation during liver transplantation as part of its ongoing interactive educational initiative. The debate focused on the difficult issue of anticoagulation during transplant surgery for prophylaxis and treatment of clots that arise during the transplant procedure. To see more join SATA.
President
M. Susan Mandell, MD, PhD
Immediate Past President
Ernesto A. Pretto, Jr. MD, MPH
President-elect
Tetsuro Sakai, MD, PhD, MHA, FASA
Secretary
Gebhard Wagener, MD
Treasurer
Lorenzo De Marchi, MD
Executive Council
Jiapeng Huang, MD, PhD, FASA, FASE
Kathirvel Subramaniam, MD, MPH, FASE
Adrian Hendrickse, BM, PgDipMEd, MAcadMEd, FRCA
Ranjit Deshpande MBBS
Newsletter Editor-in-Chief
Yong G Peng MD, PhD
Newsletter Editorial Board
Susan Mandell, MD, PhD
Jiapeng Huang, MD, PhD, FASA, FASE
Amit Bardia, MD
Sergio Navarrete, DO
David Rosenfeld, MD
Flora Simmons, MD
Natalie Smith, MD
By Sergio
More in the SATA member section…
This content is for SATA Members onlyLogin To have access to the Content! |
BOARD OF DIRECTORS: TERM 2020 – 2021President M. Susan Mandell, MD, PhD Immediate Past President President-elect Tetsuro Sakai, MD, PhD, MHA, FASA Secretary Gebhard Wagener, MD Treasurer Lorenzo De Marchi, MD Executive Council Newsletter Editor-in-Chief Newsletter Editorial Board Susan Mandell, MD, PhD |
By Sergio
Dear SATA members,
It has been a time of great reflection in the nation. The death of Mr. George Floyd ignited an outcry for immediate change. Our role as physicians and caregivers to the public has never been more important than now. We share the public’s grief at the injustice and civil unrest, but know we must remain strong because we are and will always be the ones people rely on in the most difficult times.
In these challenging times I believe there is no greater time of hope than now. We contribute by continuing our time-honored tradition of doing the most to honor and save every life; one at a time. This is our commitment to all humanity. As transplant anesthesiologists, we have a unique understanding of the purposeful work it takes to ensure every person has an equal access to all resources. We believe that every single life matters.
I send this message to all our members to thank you for the tireless work you continue to do that serves the public.
|
|
|