|
ILTS & SATA Perioperative Care in Liver Transplantation Meeting 2023
 Dear SATA Members, Residents and Fellows,
Dear SATA Members, Residents and Fellows,
The International Liver Transplantation Society (ILTS) and the Society for the Advancement of Transplant Anesthesia (SATA) are pleased to announce the first joint Perioperative Care in Liver Transplantation Meeting, which will take place on Friday, October 13, 2023, in San Francisco.
The program will feature multidisciplinary panels discussing the perioperative management of liver transplant patients, PRO/CON debates, and presentations of challenging cases.
We warmly invite you to join us in San Francisco for this event.
Dmitri Bezinover (ILTS), Gebhard Wagener (SATA)
Event Date
October 13, 2023 8:00 am – 5:00 pm
Event Location
UCSF Mission Bay Conference Center
San Francisco, California
Directions
Click here for directions from San Francisco International Airport to UCSF Mission Bay Conference Center.
Program Agenda
Click here to review the Program Agenda
Registration
Click here to register
Spring 2023 SATA Newsletter
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Winter 2023 SATA Newsletter
UNOS News
By Flora Simmons, MD
UNOS Launches National Liver Pairing Program
In an effort to increase access to living donations, UNOS has initiated a national pairing program for swapping livers. While some transplant centers have swapped livers within their own hospitals, this program now allows swapping across the nation.
Waiting Time Adjustment Approved For Kidney Transplant Candidates Affected By Race-based Calculation
After discontinuing race-based calculations for estimated glomerular filtration rate (eGFR), the new policy will now allow African-American kidney transplant candidates to receive waiting time modifications that will increase their waiting times and associated prioritization for transplant.
National Collaboration To Increase DCD Lung Transplantation Underway
UNOS recently launched a national initiative to identify and share effective practices that can increase transplantation of DCD lungs. Twenty-nine lung transplant programs are participating in this project.
Research Updates and Interesting Articles
By Michael Trostler, MD
- Validation of the Liver Transplant Risk Score in Europe
LTRS is a useful predictor of Mortality that has been validated in the United States, but not in Europe. Based on the data the European registry collects, the score has been modified to exclude Diabetes. Age, BMI, MELD score, and Dialysis status were used with linear correlation for 90-day and 1-year mortality for each point. Included 2nd article external validation of LTRS in US (2020).
Validation of the Liver Transplant Risk Score in Europe.pdf
Preoperative Stratification of Liver Transplant Recipients- Validation of LTRS.pdf
- Anesthesia Management of a Liver Transplant Recipient with Remimazolam
Case report of a 54 year old Female who had a prolonged living donor liver transplant (1037 min) and massive blood loss (22.5L) who was successfully managed with Remimazolam without recall or adverse events with EEG monitoring.
Anesthesia Management of a Liver Transplant Recipient with Remimazolam.pdf
- Survival Benefit of Living-Donor Liver Transplant
Large epidemiological study on 119,275 Liver transplant patients, with 2,820 living donor transplants which found a 13-17 year life gain for those who received a liver donor transplant for MELD>11, compared to those who stayed on the waiting list. This article generated significant interest with several comments/letters and the original authors reply which are well worth your time to read.
Survival Benefit of Living Donor Liver Transplant.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 1.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 2.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 3.pdf.
- Mortality scoring systems for liver transplant recipients: before and after model for end-stage liver disease score
An updated review article of end stage liver disease scoring systems and their inherent weaknesses. The future may be artificial intelligence, but its predictive algorithms can be individualized and may not be applicable to the wider population outside of each study cohort.
- Comprehensive quality initiative leads to immediate postoperative extubation following liver transplant
A concerted push via QA/QI project achieves safety and success for immediate extubation of liver transplant recipients in both low risk and high risk patients. There was no change in mortality and only four(1.26%) patients were reintubated within 24 hours (Total 317 patients). Quality initiative pushes immediate extubations from 13.4% to 86.7% over a five year period.
Special Topics
By Alex Stoker, MD
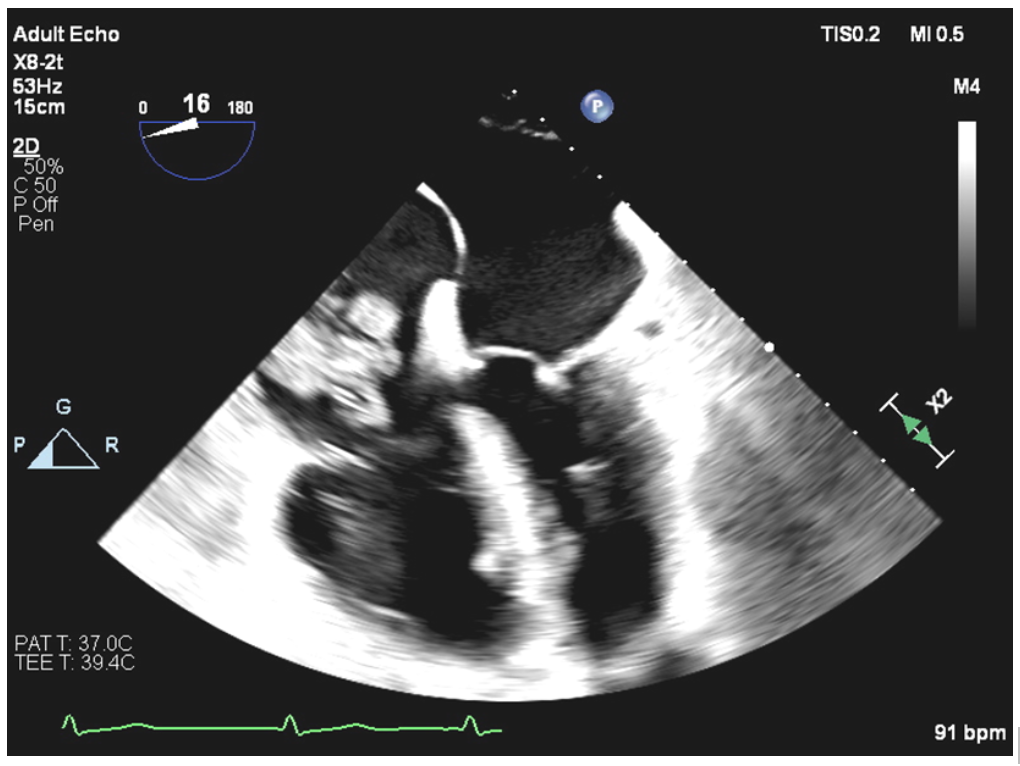
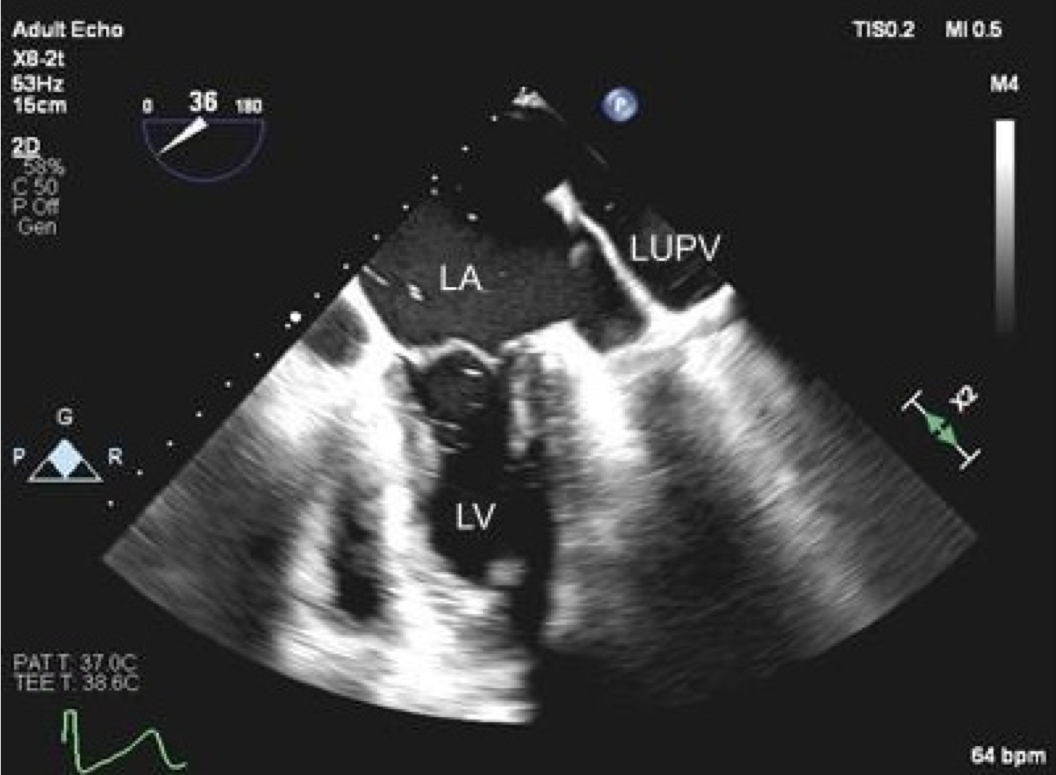
IVC stenosis during liver transplant detected with TEE
Acute inferior vena cava (IVC) stenosis after liver transplantation is a rare but significant complication that can result in liver allograft congestion and dysfunction as well as hemodynamic instability. Transesophageal echocardiography (TEE) may be used to diagnose IVC stenosis, which may reveal a high velocity or turbulent jet entering the right atrium from the IVC as detected with color flow Doppler (CFD) (see figure below). By interrogating the IVC, it may be possible to visualize the area of narrowing within the IVC, with CFD revealing flow acceleration and turbulent flow originating at the level of stenosis. Obstruction may occur in the suprahepatic IVC, infrahepatic IVC or hepatic veins and can be due to surgical complication or due to thrombosis. There is increasing use of TEE to evaluate hepatic and IVC vasculature during liver transplantation (Khurmi et al, 2019). Reference
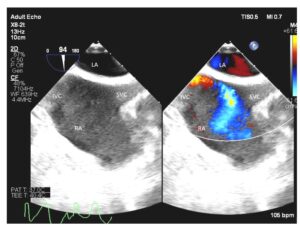 Midesophageal bicaval view with color compare showing the image both with and without color flow Doppler. A turbulent and high velocity jet is seen entering the right atrium from the IVC due to IVC stenosis. LA, left atrium; RA, right atrium; IVC, inferior vena cava; SVC, superior vena cava.
Midesophageal bicaval view with color compare showing the image both with and without color flow Doppler. A turbulent and high velocity jet is seen entering the right atrium from the IVC due to IVC stenosis. LA, left atrium; RA, right atrium; IVC, inferior vena cava; SVC, superior vena cava.
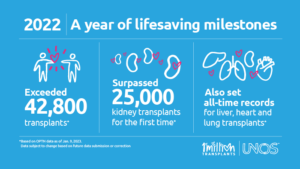
2022 UNOS Organ Transplant Summary
By Alexandra Ruan, MD
https://unos.org/news/2022-organ-transplants-again-set-annual-records/
- More than 42,800 organ transplants performed in 2022, a 3.7% increase from 2021
- Total kidney transplants exceeded 25,000 for the first year ever
- Annual records also set for liver (9,528), heart (4,111) and lung (2,692) transplants
- Over 6,400 living donor transplants
- Deceased donation increased for 12th consecutive year
- The U.S. has now performed over 1 million transplants
In the Spotlight: Virginia Commonwealth University (VCU) Health System – Hume/Lee Transplant Center
By David Rosenfeld, MD, FASA
For this winter’s section we reached out to Spencer Liebman, MD, who is Chief, Division of Transplant Anesthesiology at VCU. Formerly known as Medical College of Virginia, VCU is an 820 bed health system and one of the nation’s first transplant programs. This historic program is named for David M. Hume, MD and Hyung Mo Lee, MD, and is where one of the earliest identical twin kidney transplants was performed in 1957, with the overall program starting in 1962. Soon after livers began in 1964, with the world’s 16th heart transplant in 1968. The scope of organs includes livers, kidneys, pancreas, and hearts, with experience in combined heart-liver transplant. A total of 502 organs were transplanted in 2022.
VCU offers 112 ICU beds, 16 of which are cardiac, and a dedicated transplant ICU growing to 10 beds under the direction of Megan Rashid, MD. The liver practice is large with 168 total adult organs, 21 of which were from living donors. Staffing is in a team care model with five dedicated attendings, six specially trained CRNAs, and residents rotating in their CA2/CA3 years. TEG is universal, and TEE is utilized for greater than 80% of cases. As is becoming more common, intraoperative hemodialysis (not CRRT) was used in 40% of cases in 2022. They offer a unique Active Severe Alcoholic Hepatitis Transplant Program with support services and strategies in place. VCU has a non-ACGME liver fellowship with a hybrid model of combined fellow and faculty time and two positions per year. In 2016 the Total Pancreatectomy with Islet Cell Autotransplant (TPIAT) program was started with the addition of Transplant Surgeon Marlon Levy, MD to the faculty. A total of 18 TPIATs were performed in 2022 for chronic pancreatitis, and they are one of the few centers offering this experimental therapy. Their cardiac program is the longest running on the east coast and the second oldest in the US. Over 680 heart transplants have been performed, and they offer an ACGME accredited Adult Cardiothoracic Anesthesiology fellowship with two fellows per year. There are no lung transplants being performed at present.
Many thanks to Dr. Liebman for sharing details of the transplantation program at VCU. If interested in having your program highlighted in the future, please contact David Rosenfeld, Mayo Clinic Arizona at Rosenfeld.david@mayo.edu
*The original newsletter identified VCU as performing the first identical twin kidney transplant in 1957. This was in error, the first kidney transplant was performed in an identical twin by Dr Joseph E.Murray in Boston in 1954. Correction made above.
Report from the Executive Council
By Susan Mandell, MD
We look forward to seeing SATA members at the in person SATA National Meeting, held at the IARS on April 17th, 2023, in Denver Colorado. Please remember to renew your membership for free entry to the meeting. SATA is pleased to announce it will hold the first combined meeting with the International Liver Transplant Society-SATA meeting just prior to the ASA in San Francisco. This has been a very popular meeting and well attended.
The Council is pleased to announce that there are now seven regional SATA meetings. Please check for the meeting closest to you. Service on the SATA Accessibility and Diversity Committee is now open to all members. The Vanguard committee has been revitalized and membership is open to all faculty who are within 5 years of residency completion or are younger than 42, please reach out to the SATA Office for more information.
Announcements
We are pleased to announce that SATA will be represented at the 10th Annual Korean Society of Transplant Anesthesiologists (KSTA) meeting in Seoul, Korea. During the Joint KSTA-SATA session (March 18, 2023 11:20-12:50 KST), moderated by Dr. Tetsuro Sakai and Justin Sangwook Ko, Dr. Satish Kumar will present on emerging evidence for coronary artery disease screening in liver transplant candidates and Dr. Ramona Nicolau-Raducu will present on post-reperfusion hyperfibrinolysis.
SATA is delighted to endorse the first International Symposium for Abdominal Organ Transplant (ISAOT) in Santiago, Chile, June 8-9, 2023.
This opportunity is presented by Dr. Klaus Torp at Mayo Clinic-Jacksonville (Founding member of SATA) who has supported the physician exchange program with the Clinica Alemanha in Santiago de Chile. Dr. Lucile Gignon (Faculty Anesthesiologist at the Clinica Alemanha in Santiago de Chile) is the local organizer of the meeting.
Attention liver transplant anesthesiologists and program directors! SATA is offering free 6 month membership to fellows! Please sign up by emailing sata@pacainc.com. We look forward to welcoming new fellow members!
Join the Vanguard Committee ***
Transplant Anesthesia Upcoming Meetings
SATA Meetings
SATA Tristate Regional Meeting – in person and virtual
March 25th, 2023, New York, NY
April 17th, 2023, Denver, CO
Other Meetings:
The 10th annual scientific meeting of the Korean Society of Transplantation Anesthesiologists (KSTA), March 18th, Seoul, Korea – in person and hybrid
Joint KSTA-SATA Session: 11:20 – 12:50 KST
IARS/AUA/SOCCA Annual Meeting – in person and hybrid
April 13-16th, 2023, Denver, CO
The 2023 International Congress of ILTS, ELITA and LICAGE
May 3-6, 2023; Rotterdam, Netherlands
American Transplant Congress (ATC) 2023 Annual Meeting
June 3-7, 2023, San Diego, CA
International Symposium for Abdominal Organ Transplant (ISAOT)
June 8-9, 2023, Santiago, Chile
Tristate Regional Transplant Anesthesiology Conference 2023
Learning objectives – On completion of this activity the participants will be able to
- Learn about the concept of frailty and its importance in evaluation/management and outcomes for abdominal transplant recipients
- Discuss indications and practical considerations for use of veno-venous bypass in liver transplantation and advanced hepatobiliary surgery
- Review strategies for prevention and treatment of acute kidney injury in liver transplantation
- Learn about strategies to improve graft quality in donation after circulatory determination of death in organ transplantation, including machine perfusion
- Review ethical and practical considerations in organ donation after circulatory determination of death
- Discuss administrative considerations in managing a transplant anesthesiology service line and fellowship
Target audience
Transplant anesthesiologists, intensivists, transplant surgeons, residents, and fellows.
Time and Location:
SATURDAY, MARCH 25TH, 2023: 9 AM – 2 PM, WEILL CORNELL MEDICINE
1300 YORK AVENUE, NEW YORK, NY 10065 WEILL AUDITORIUM (C-200)
Virtual Venue:
https://weillcornell.zoom.us/j/97750761082?from=addon
Meeting ID: 977 5076 1082
Schedule:
9:00 – 9:30: Breakfast and Welcome: Christine Lennon M.D., Weill Cornell Medicine
9:30 – 10:30: Perioperative considerations
Frailty in abdominal transplant – Joseph Scarpa, M.D. and Rohan Panchamia M.D., Weill Cornell Medicine
Veno-venous bypass in liver transplantation – Juan Rocca M.D., Weill Cornell Medicine
ICU Management: postoperative acute kidney injury in liver transplantation – Christopher Tam M.D., Montefiore Medical Center
10:30 – 10:45: Break
10:45 – 11:30: Donor considerations
DCD donation and NRP – Zeeshan Akhtar M.D., The Mount Sinai Hospital
DCD practical and ethical considerations – Christine Lennon M.D., Weill Cornell Medicine
11:30 – 12:15: Lunch
12:15 – 1:15: Administrative considerations
Anesthesiologist as the perioperative physician: the transplant anesthesiology model – Nikhil Chawla M.D., Yale New Haven Hospital
Transplant anesthesiology service considerations – Joseph Yeh M.D., NYU Langone Health
Transplant anesthesiology fellowship considerations – Natalie Smith M.D., The Mount Sinai Hospital
1:15 – 1:45: Keynote address: Tetsuro Sakai M.D., University of Pittsburgh Medical Center
1:45 – 2:00 Closing Remarks: Gebhard Wagener M.D., Columbia University Irving Medical Center
Registration Fees and Link:
Complimentary Registration if no CME credits are required
$30.00 for SATA and SCA Members – CME Credits Needed
$60.00 for Non-SATA and SCA Members – CME Credits Needed
https://sata2022.wufoo.com/forms/zid5tgc0d8hdb3/
Organizing committee members (alphabetical):
- Ranjit Deshpande, MD, FCCM (Yale New Haven Hospital, New Haven, CT)
- Christine Lennon, MD (Weill Cornell Medicine, New York, NY)
- Marina Moguilevitch, MD (Montefiore Medical Center, Bronx, NY)
- Natalie Smith, MD (The Mount Sinai Hospital, New York, NY)
- Gebhard Wagener, MD (Columbia University Irving Medical Center, New York, NY)
- Joseph Yeh, (NYU Langone Health, New York, NY)
Directions to Weill Auditorium (C-200)
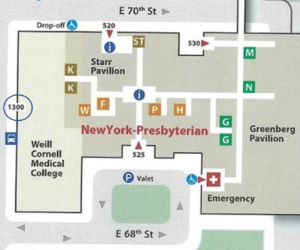 Enter the medical school at 1300 York Avenue.
Enter the medical school at 1300 York Avenue.
After you go through security, proceed to the second floor via the stairs or elevator.
As you exit the staircase, make a left and walk down the hall. C-200 will be on the right.
2023 DMV Regional SATA Meeting
Program overview:
This SATA regional meeting will provide discussion of novel areas of interest in liver, heart, and lung
transplantation.
Learning objectives:
At the end of this session participants will be able to:
1. Determine the potential benefits and challenges of ECMO in liver, heart and lung transplantation
2. Understand risk and benefit of postponing abdominal closure after liver transplantation
3. Learn the different antimicrobial strategies adopted in abdominal and cardio-thoracic transplant
patients to protect them from infection in the perioperative period
4. Understand the potential complication of vascular cannulation for V-V bypass
5. Understand the challenges of managing blood products reserve for a patient with antibody
6. Determine the best approach to liver transplant for a patient with Severe AS
Target audience:
Anesthesiologists, Intensivists, Surgeons, Hepatologists, Cardiologists, Fellows,
Resident, Medical Students, Nurse anesthetists, Advanced Practice Nurses, Anesthesiologist Assistants,
Physician Assistants, and Nursing staff who are involved in the perioperative care of transplant patients.
Core Faculty
Lorenzo De Marchi, MD, FASE (Chair)
Professor of Clinical Anesthesia
MedStar-Georgetown University Hospital
Aliaksei Pustavoitau, MD, MHS, FCCM
Associate Professor of Anesthesiology and Critical Care Medicine
Johns Hopkins University
Katie Forkin, MD
Associate Professor of Anesthesiology
Division Chief, Liver Transplant Anesthesia
University of Virginia Health
Sergio Navarrete, DO
Assistant Professor
Virginia Commonwealth University
Additional Faculty listing:
Promise Ariyo, MD MPH
Assistant Professor
Divisions of Cardiac Anesthesia & Critical Care
Department of Anesthesiology & Critical Care Medicine
Johns Hopkins University
Zachary Janik, MD
Anesthesia Resident
Johns Hopkins University School of Medicine
Olivia S. Kates, MD
Assistant Professor of Medicine
Johns Hopkins University
Shane Ottman, MD
Assistant Professor of Surgery
Johns Hopkins University
Pedjman Radkani, MD
Assistant Professor of Surgery
MedStar-Georgetown University Hospital
Gregory Serrao, MD, MSE, FACC, FSCAI
Director, Mechanical Circulatory Support
Cardiac Catheterization Laboratory
Icahn School of Medicine at Mount Sinai
Benjamin Wilson, MD
Anesthesia Resident
MedStar-Georgetown University Hospital
Hamy Kassahun, MD
Anesthesia Resident
University of Virginia Health
SATA-DMV 2023 10:25 am – 3:30 pm
10:25 am – 10:30 am Welcome and Introduction – Lorenzo De Marchi, MD (MGUH)
10:30 am -11:20 am ECMO in Transplant – Moderator: Aliaksei Pustavoitau, MD (JHH)
10:30 am – 10:50 am ECMO in liver transplant – Gregory Serrao, MD (Mount Sinai)
10:50 am – 11:10 am ECMO in CT transplant – Promise Ariyo, MD (JHH)
11:10 am – 11:20 am Q&A
11:20 am – 11:30 am Presidential address
11:30 am – 11:35 am Break
11:35 am – 12:30 pm Management of open abdomen in Liver Transplant (Pro/ Con) – Moderator: Sergio Navarrete, DO (VCU)
11:35 am – 11:55 am Con – Pejman Radkani, MD (MGUH)
11:55 am – 12:15 pm Pro – Shane Ottmann, MD (JHH)
12:15 am – 12:35 pm The CCM Perspective – Aliaksei Pustavoitau (JHH)
12:35 pm – 12:50 pm Q&A
12:50 pm – 1:30 pm Lunch break
1:30 pm – 2:20 pm Third Session – Moderator: Lorenzo De Marchi, MD (MGUH)
1:50 pm – 2:10 pm Perioperative Antimicrobial Therapy in Abdominal Transplant – Olivia Kates, MD (JHH)
2:10 pm – 2:20 pm Q&A
2:20 pm – 2:30 pm Break
2:30 pm – 3:25 pm Challenging Cases – Moderator: Katherine Forkin, MD (UVA)
2:30 pm – 2:45 pm LDLT in a patient with Severe AS – Hamy Kassahun , MD (UVA)
2:45 pm – 3:00 pm Blood management for patients with antibodies-Zachary Janik,MD (JHH)
3:00 pm – 3:15 pm Complication V-V bypass cannulation – Ben Wilson, MD (MGUH)
3:15 pm – 3:25pm Q&A
3:25 pm – 3:30 pm Closing Remarks
The 2023 Symposium of the Society for the Advancement of Transplant Anesthesia
In conjunction with the annual meeting of the International Anesthesia Research Society (IARS)
Note: SATA Council meeting on April 16
Monday April 17, 2023 (8 AM – 3:00 PM)
Location: Mineral A-C room on Level 3, Hyatt Regency Denver at Colorado Convention Center, 650 15th Street, Denver, CO 80202
Registration (with CME credit):
https://sata2022.wufoo.com/forms/z1e9i2pz1p5x4o8/ or https://tinyurl.com/mr2rn9ks
$50 for SATA, SOCCA and SCA members, $150 for non-members, free for trainees
7:30 am – 8:00 am Registration
8:00 am – 8:15 am Welcome and Introduction
- Gebhard Wagener, President-elect – Columbia University, New York, NY
8:15 am – 9:15 am: Session 1: The Yin and Yang of coagulation (60 min)
Moderator: Alexandra Ruan – Stanford University, Stanford, CA
- New models and new drugs in coagulation (20-25 min)
- Art Bracey – Baylor College of Medicine
- Anticoagulants and surgery: Stop, continue, reverse?
- Abdominal transplant (10 min)
- Manoj Iyer – The Ohio State University Wexner Medical Center
- Thoracic transplant (SCA) (10 min)
- Kenichi Tanaka – The University of Oklahoma College of Medicine
- Abdominal transplant (10 min)
9:15 am – 9:45 am: Coagulation debate (30 min)
- Are ROTEM and Cryoprecipitate dangerous for liver transplants? (10 min)
- Christine Nguyen-Buckley – University of California Los Angeles
- Are PCC and Vit K dangerous for heart transplants? (10 min)
- Jiapeng Huang – University of Louisville, Kentucky
9:45 am – 10:30 am: Session 2: Pain and analgesia for transplant surgeries (45 min)
- Regional techniques for thoracic transplants and VADs (10 min)
- Anis Dizdarevic – Columbia University, New York, NY
- Indications and challenges to early extubation in the operating room (10 min)
- Courtney Scott – Mayo Clinic Jacksonville, FL
- Analgesia for living liver donors (KSA) (15 min)
- Justin Ko – Sungkyunkwan University School of Medicine, Samsung Medical Center; Director of Scientific Affairs, Korean Society of Anesthesiologists – Seoul, Korea
10:30 am – 11:00 am: Break
11:00 am – 11:20 am State of the Society
- Ted Sakai, President of SATA – University of Pittsburgh Medical Center, PA
- (Introduction: Susan Mandell – McGovern Medical Center, Houston TX
11:20 am – 12:00 pm Case presentations
Moderator: Adrian Hendrickse – University of Colorado Denver, CO
- Thoracic Transplant
- Michelle Chen- Columbia University, New York, NY
- Mentor: Andrea Miltiades – Columbia University, New York, NY
- Abdominal transplant
- Zach Fleissner – Mayo Clinic Jacksonville, FL
- Mentor: Ryan Chadha – Mayo Clinic Jacksonville, FL
12:00 pm – 1:00 pm Session: What’s new in organ donation and allocation (60 min)
- How is transplantation organized: past and future of UNOS and organ transplantation in the US (15-20 min)
- Jennifer Prinz – CEO of Donor Alliance and Vice Chair of the OPTN Policy Committee
- The impact of the new regulation of organ allocation on transplant practices (15-20 min)
- Jim Pompeselli – University of Colorado Denver, CO
- Deceased donor management and machine perfusion modalities (15 min)
- Emily Vail – University of Pennsylvania, Philadelphia, PA
1:00 pm – 1:30 pm Break
1:30 pm – 2:30 Session: How and why do we maintain blood pressure and perfusion (45 min)
Moderator: Ana Fernandez-Bustamante – University of Colorado Denver, CO
- Just a bystander organ? How do we protect the kidney? (15 min)
- HT Lee – Columbia University, New York, NY
- New kids on the block
- Angiotensin (10 min)
- Michael Bokoch – University of California San Francisco, CA
- Terlipressin (in collaboration with the Society of Critical Care Anesthesiologist, SOCCA) (10 min)
- Sathish Kumar, University of Michigan, Ann Arbor, MI
- Angiotensin (10 min)
2:30 pm – 2:45 pm First SATA Research Award
- SATA Research Committee
- She- Lu Pai – Mayo Clinic Jacksonville, FL
- Dieter Adelmann – University of California San Francisco, CA
2:45 pm – 3:00 pm Closing Remarks
- Lorenzo De Marchi, SATA Secretary – MedStar Georgetown University Hospital
December 2022 Article of the Month
Alcohol-associated liver disease predicts increased post-liver transplant opioid use.
Abstract:
BACKGROUND: Alcohol-associated liver disease (ALD) is a rising indication for liver transplantation (LT). Prolonged opioid use after LT leads to increased graft loss and mortality. The aim is to determine if patients transplanted with a primary diagnosis of ALD had higher risk of post-LT opioid use (p-LTOU) compared to non-ALD patients.
METHODS: This is a retrospective study of patients who underwent LT between 2015 and 2018 at Medstar Georgetown Transplant Institute. Patients with prolonged hospitalization post-LT (>90 days), death within 90 days post-LT, and re-transplants were excluded.
RESULTS: Two hundred and ninety-seven patients were transplanted, among 29% for indications of ALD. ALD patients were younger (52 vs. 56 years), more likely to be male (76% vs. 61%), Caucasian (71% vs. 44%), have higher MELD (28.8+/-8.8 vs. 25+/-8.8), and psychiatric disease than non-ALD patients (P < .05). There was no difference in pre-LT use of opioids, tobacco, marijuana, or illicit drugs between ALD and non-ALD patients. Pre-LT opioid use (OR = 11.7, P < .001), ALD (OR = 2.5, P = .01), and MELD score (OR = .95, P = .02) independently predicted 90-day p-LTOU.
CONCLUSIONS: ALD, pre-LT opioid use, and MELD score independently predict p-LTOU. Special attention should be paid to identify post-LT prolonged opioid use in ALD patients.
Comments made by Cale Kassel M.D., FASA
Summary:
In this retrospective study, the Johnson-Laghi et al reviewed patients undergoing liver transplantation focusing on patients with known alcoholic liver disease and previous opioid use prior to transplantation. As has been described, the use of pre-operative opioids is associated with worse outcomes in other surgical procedures. The authors sought to identify if post-LT opioid use (p-LTOU) was greater in patients with alcoholic liver disease (ALD) compared to those without alcoholic liver disease.
Patient demographic data included diagnosis of psychiatric disease, use of psychiatric medications, use of illicit drugs, use of benzodiazepines, use of marijuana, prior alcoholic rehabilitation, and legal encounters related to alcohol (DUI). Use of pre-operative opioids included use both scheduled and as needed within the three months prior to transplantation. The total dose was converted to morphine equivalents for comparison.
Overall, opioid use post-LT was more common with patients with ALD compared to those without at 30, 60, and 90 days. At 90 days, 44% of ALD patients were taking opioids compared to 27% of non-ALD patients (p = 0.004). Multi-variate logistic regression demonstrated pre-LT opioid use, primary diagnosis of ALD, and lower MELD predicted 90-day post-LT opioid use.
Further analysis showed specific risk factors for p-LTOU at 60 days to include living alone. As the authors noted, this shows the importance of good social support for patients evaluated for LT. This was not a significant variable at 90 days however.
As the authors noted, more research is needed on this topic to further identify risk factors for opioid use following LT. Additionally, this is an area for anesthesiologist involved in the listing process to add value. Opioid tapering prior to LT may provide benefit for patients. Identifying patients with any patient who take opioids, can allow for early intervention including opioid tapering.
Fall 2022 Newsletter
Research Updates and Interesting Articles
Michael Trostler, MD
Highlights: South Korean study of 398 patients evaluating incidence of post-reperfusion syndrome in a propofol vs sevoflurane anesthetic, found a statistically significant decrease in the sevoflurane group.
2. Outcomes of Bariatric Surgery Before, During, and After Solid Organ Transplantation
Highlights: Bariatric surgery was able to be performed safely, pre-transplant, simultaneously with transplant, or post-transplant with no increase in adverse events related to the bariatric procedure. Bariatric surgery leads to weight loss and decreased comorbidities in this patient population.
3. Orthotopic Transplantation of the Full-length Porcine Intestine After Normothermic Machine Perfusion
Highlights: The new trend of machine perfusion in organ transplantation is at the forefront of transplantation and extended criteria organs. Porcine model of intestinal transplant has been shown to be viable and successful.
Highlights: A review article of 9 studies including 2000 patients shows no increase in disease free survival, HCC recurrence or impaired overall survival. If cell salvage is desired, it should not be immediately disregarded as an option just because of a hepatocellular carcinoma diagnosis.
Highlights: After a peak in living donor liver transplants in 2001 there was a fall, but there has been a steady rise from 2011 to 2019. There have been improvements in transplant survival over the years with a significantly decreased mortality over the past few years compared to the first few years.
|
|
In the Spotlight: Saint Louis University Medical Center Transplant Program
For this quarter’s segment, we connected with Dr. Govind Rangrass, MD, Director of Transplant Anesthesia and Director of Quality/Patient Safety at the new 400-bed SSM Health/Saint Louis University Hospital (SLUH).
Saint Louis University has a long history with abdominal transplant, at one time being one of the busiest transplant centers in the country. In recent years, their volumes have hovered between 30-40 liver transplants/year. SLUH recently merged with the SSM Health, a large hospital network, and as its only transplant center, the program is gearing up for an increase in transplant evaluations and referrals and is carefully navigating the listing process for high-risk patients.
As part of the selection process, the transplant anesthesia director sits on the Liver Recipient Selection Committee. A unique aspect of their program is that they have a separate High Risk Cardiac Evaluation Meeting, which meets weekly to discuss candidates with complex cardiac disease who may benefit from additional pre transplant work-up optimization and ensure postoperative continuity of care with the cardiology team. One of their transplant faculty was the corresponding author of the newly released AHA Scientific Statement on Coronary Heart Disease Screening in Kidney and Liver Transplantation Candidates published in Circulation. Between 2019-2021, patients undergoing liver transplantation at SSM Health/SLUH had 100% survival at one month and 94% survival at one year post transplant.
Their program is one of the few that uses alternative portal flow in transplant for patients with portal vein thrombosis using reno-portal (connecting left renal vein of recipient to donor portal vein to act as inflow) and gastro-portal (using left gastric vein as inflow) anastomoses. Another unique aspect of the program is the disproportionately high number of hepatitis C positive donor livers utilized (~20%). Their program is gaining more experience with the Transmedic normothermic perfusion pumps, which it intends to continue using in the future.
TEG 6S is routinely used and available and housed in the hospital coagulation lab, with a real time tracing available in the operating room. Venovenous bypass is used selectively for redo liver transplants, patients with portopulmonary hypertension with RV dysfunction or hepatopulmonary syndrome, and high MELD patients on preoperative CRRT. Heparin (50U/kg) is administered for hypercoagulable patients prior to caval cross-clamping, and antifibrinolytics are administered as a bolus during the anhepatic stage. Octreotide infusions (50mcg bolus followed by 100mcg/hr) are routinely run for patients with significant portal hypertension.
The SSM Health/SLUH transplant program hosts a robust outcomes research center and has multiple grant-funded research projects. Examples include a study on biomarkers of kidney function to predict perioperative acute kidney injury; a normothermic perfusion basic science lab studying pharmacologic tools to reduce ischemia reperfusion injury in discarded human livers placed on perfusion pumps; and a $1.8 million grant in conjunction with Missouri University of Science and Technology to develop artificial intelligence driven decision-making tools for organ allocation.
Announcements
The Accessibility and Inclusion Committee
The SATA Council is pleased to announce the introduction of The Accessibility and Inclusion Committee. The Committee will help develop SATA policies by providing the Council with their views on how to ensure members have equal access to all service opportunities within the organization, All SATA members are invited to nominate themselves or a colleague to serve on this new important committee as part of the society leadership. Please send your nominations to the SATA Secretary: Lorenzo De Marchi at demarchilorenzo@yahoo.com
Service: Appointment by SATA Council
Term: 2 years; can be renewed
Requirements: SATA Membership in good standing
Purpose: Oversight and Advocacy Committee
Seed Grant Funding Mechanism
The SATA Seed Grant is a one-year $5,000 transplant project starter grant, open to junior faculty members and trainee physician members of the Society. The grant aims to inspire and assist aspiring faculty/trainee physicians who have yet to receive any previous funding to start a transplant-related project. The grant requires the recipient to submit a support letter from the mentoring faculty and the Department Chairperson.
Application/Grant Cycle:
-
November 1, 2022 – Announcement of the grant
-
December 1, 2022 – Opening of the submission site
-
February 28, 2023 – Closure of submission site
-
April 1, 2023 – Announcement of the awardee and send letters of feedback to the other applicants
-
April 17, 2023 – Grant presentation at SATA National Meeting in Denver, CO
-
July 1, 2023 – Grant initiation
-
December 31, 2023 – submission of the mid-term report
-
June 30, 2023 – submission of the final report
Click here to review the SATA Seed Grant Grading
Click here to review the SATA Seed Grant Proposal
Transplant Anesthesia Upcoming Meetings
SATA Meetings
Southeastern SATA Regional Meeting: November 5, 2022
SATA West Meeting: December 10, 2022, San Francisco – in person and hybrid.
Submit an Abstract by email to: Dieter.Adelmann@ucsf.edu
Mid-Western SATA Regional Meeting: January 21, 2023
Other Meetings:
The Liver Meeting – aasld.org, November 4-8, 2022, Washington, DC
The 2023 International Congress of ILTS, ELITA and LICAGE
May 3-6, 2023; Rotterdam, Netherlands
American Transplant Congress (ATC) 2023 Annual Meeting
June 3-7, 2023, San Diego, CA
October 2022 Article of the Month
Utilization and outcomes of deceased donor SARS-CoV-2–positive organs for solid organ transplantation in the United States.
Abstract:
Coronavirus disease-19 has had a marked impact on the transplant population and processes of care for transplant centers and organ allocation. Several single-center studies have reported successful utilization of deceased donors with positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) tests. Our aims were to characterize testing, organ utilization, and transplant outcomes with donor SARS-CoV-2 status in the United States. We used Scientific Registry of Transplant Recipients data from March 12, 2020 to August 31, 2021 including a custom file with SARS-CoV-2 testing data. There were 35 347 donor specimen SARS-CoV-2 tests, 77.5% upper respiratory samples, 94.6% polymerase chain reaction tests, and 1.2% SARS-CoV-2-positive tests. Donor age, gender, history of hypertension, and diabetes were similar by SARS-CoV-2 status, while positive SARS-CoV-2 donors were more likely African-American, Hispanic, and donors after cardiac death (p-values <.01). Recipient demographic characteristics were similar by donor SARS CoV-2 status. Adjusted donor kidney discard (odds ratio = 2.08, 95% confidence interval [CI] 1.66-2.61) was higher for SARS-CoV-2-positive donors while donor liver (odds ratio = 0.44, 95% CI 0.33-0.60) and heart recovery (odds ratio = 0.44, 95% CI 0.31-0.63) were significantly reduced. Overall post-transplant graft survival for kidney, liver, and heart recipients was comparable by donor SARS-CoV-2 status. Cumulatively, there has been significantly lower utilization of SARS-CoV-2 donors with no evidence of reduced recipient graft survival with variations in practice over time.
Comments made by Cale Kassel M.D., FASA
Summary:
When the COVID-19 pandemic began, there were obvious concerns among the transplant community. First and foremost, how could we protect patients following transplant and while waiting from transplant. As our understanding of COVID-19 evolved, so to did our ability to manage the disease in organ transplantation. The question of utilizing COVID-positive organs for transplantation emerged. Schold, et al reviewed SRTR data to look at utilization of COVID-positive organs (kidney, liver, and heart) from early in the pandemic to present. Several key findings emerged as they evaluated the data.
First, they found utilizing COVID-positive grafts did not demonstrate worse outcomes for patients. Graft survival was similar between COVID-positive and COVID-negative grafts for kidney (95.5% vs. 95.3%), liver (93.9% vs. 97.0%), and heart (92.8% vs. 96.7%).
Second, utilization of COVID-positive donors remained low. Recovery of COVID-positive organs was lower for kidneys, livers, and hearts. Additionally, discard of recovered grafts were lower in COVID-positive grafts. However, kidney graft discard rate of COVID-positive grafts was lower in the later study period (Dec 2020-April 2021) compared to the early study period (March 2020-November 2020). The overall rate of discard for COVID-positive kidneys was still lower than COVID-negative. Heart and liver discard rates were lower in COVID-positive donors as well.
As we continue to learn more about the effect of transplantation of COVID-positive organs, we can continue to optimize patients and grafts to improve outcomes. Early data from this study and others suggests COVID-positive grafts can provide a safe option for patients awaiting transplantation.
References:
Schold JD, Koval CE, Wee A, Eltemamy M, Poggio ED. Utilization and outcomes of deceased donor SARS-CoV-2–positive organs for solid organ transplantation in the United States. American Journal of Transplantation 2022;22(9):2217-2227. DOI: https://doi.org/10.1111/ajt.17126.