UNOS News
By Flora Simmons, MD
UNOS Launches National Liver Pairing Program
In an effort to increase access to living donations, UNOS has initiated a national pairing program for swapping livers. While some transplant centers have swapped livers within their own hospitals, this program now allows swapping across the nation.
Waiting Time Adjustment Approved For Kidney Transplant Candidates Affected By Race-based Calculation
After discontinuing race-based calculations for estimated glomerular filtration rate (eGFR), the new policy will now allow African-American kidney transplant candidates to receive waiting time modifications that will increase their waiting times and associated prioritization for transplant.
National Collaboration To Increase DCD Lung Transplantation Underway
UNOS recently launched a national initiative to identify and share effective practices that can increase transplantation of DCD lungs. Twenty-nine lung transplant programs are participating in this project.
Research Updates and Interesting Articles
By Michael Trostler, MD
- Validation of the Liver Transplant Risk Score in Europe
LTRS is a useful predictor of Mortality that has been validated in the United States, but not in Europe. Based on the data the European registry collects, the score has been modified to exclude Diabetes. Age, BMI, MELD score, and Dialysis status were used with linear correlation for 90-day and 1-year mortality for each point. Included 2nd article external validation of LTRS in US (2020).
Validation of the Liver Transplant Risk Score in Europe.pdf
Preoperative Stratification of Liver Transplant Recipients- Validation of LTRS.pdf
- Anesthesia Management of a Liver Transplant Recipient with Remimazolam
Case report of a 54 year old Female who had a prolonged living donor liver transplant (1037 min) and massive blood loss (22.5L) who was successfully managed with Remimazolam without recall or adverse events with EEG monitoring.
Anesthesia Management of a Liver Transplant Recipient with Remimazolam.pdf
- Survival Benefit of Living-Donor Liver Transplant
Large epidemiological study on 119,275 Liver transplant patients, with 2,820 living donor transplants which found a 13-17 year life gain for those who received a liver donor transplant for MELD>11, compared to those who stayed on the waiting list. This article generated significant interest with several comments/letters and the original authors reply which are well worth your time to read.
Survival Benefit of Living Donor Liver Transplant.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 1.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 2.pdf
Reply to Survival Benefit of Living Donor Liver Transplant 3.pdf.
- Mortality scoring systems for liver transplant recipients: before and after model for end-stage liver disease score
An updated review article of end stage liver disease scoring systems and their inherent weaknesses. The future may be artificial intelligence, but its predictive algorithms can be individualized and may not be applicable to the wider population outside of each study cohort.
- Comprehensive quality initiative leads to immediate postoperative extubation following liver transplant
A concerted push via QA/QI project achieves safety and success for immediate extubation of liver transplant recipients in both low risk and high risk patients. There was no change in mortality and only four(1.26%) patients were reintubated within 24 hours (Total 317 patients). Quality initiative pushes immediate extubations from 13.4% to 86.7% over a five year period.
Special Topics
By Alex Stoker, MD
IVC stenosis during liver transplant detected with TEE
Acute inferior vena cava (IVC) stenosis after liver transplantation is a rare but significant complication that can result in liver allograft congestion and dysfunction as well as hemodynamic instability. Transesophageal echocardiography (TEE) may be used to diagnose IVC stenosis, which may reveal a high velocity or turbulent jet entering the right atrium from the IVC as detected with color flow Doppler (CFD) (see figure below). By interrogating the IVC, it may be possible to visualize the area of narrowing within the IVC, with CFD revealing flow acceleration and turbulent flow originating at the level of stenosis. Obstruction may occur in the suprahepatic IVC, infrahepatic IVC or hepatic veins and can be due to surgical complication or due to thrombosis. There is increasing use of TEE to evaluate hepatic and IVC vasculature during liver transplantation (Khurmi et al, 2019). Reference
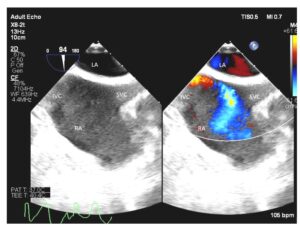 Midesophageal bicaval view with color compare showing the image both with and without color flow Doppler. A turbulent and high velocity jet is seen entering the right atrium from the IVC due to IVC stenosis. LA, left atrium; RA, right atrium; IVC, inferior vena cava; SVC, superior vena cava.
Midesophageal bicaval view with color compare showing the image both with and without color flow Doppler. A turbulent and high velocity jet is seen entering the right atrium from the IVC due to IVC stenosis. LA, left atrium; RA, right atrium; IVC, inferior vena cava; SVC, superior vena cava.
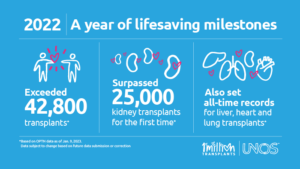
2022 UNOS Organ Transplant Summary
By Alexandra Ruan, MD
https://unos.org/news/2022-organ-transplants-again-set-annual-records/
- More than 42,800 organ transplants performed in 2022, a 3.7% increase from 2021
- Total kidney transplants exceeded 25,000 for the first year ever
- Annual records also set for liver (9,528), heart (4,111) and lung (2,692) transplants
- Over 6,400 living donor transplants
- Deceased donation increased for 12th consecutive year
- The U.S. has now performed over 1 million transplants
In the Spotlight: Virginia Commonwealth University (VCU) Health System – Hume/Lee Transplant Center
By David Rosenfeld, MD, FASA
For this winter’s section we reached out to Spencer Liebman, MD, who is Chief, Division of Transplant Anesthesiology at VCU. Formerly known as Medical College of Virginia, VCU is an 820 bed health system and one of the nation’s first transplant programs. This historic program is named for David M. Hume, MD and Hyung Mo Lee, MD, and is where one of the earliest identical twin kidney transplants was performed in 1957, with the overall program starting in 1962. Soon after livers began in 1964, with the world’s 16th heart transplant in 1968. The scope of organs includes livers, kidneys, pancreas, and hearts, with experience in combined heart-liver transplant. A total of 502 organs were transplanted in 2022.
VCU offers 112 ICU beds, 16 of which are cardiac, and a dedicated transplant ICU growing to 10 beds under the direction of Megan Rashid, MD. The liver practice is large with 168 total adult organs, 21 of which were from living donors. Staffing is in a team care model with five dedicated attendings, six specially trained CRNAs, and residents rotating in their CA2/CA3 years. TEG is universal, and TEE is utilized for greater than 80% of cases. As is becoming more common, intraoperative hemodialysis (not CRRT) was used in 40% of cases in 2022. They offer a unique Active Severe Alcoholic Hepatitis Transplant Program with support services and strategies in place. VCU has a non-ACGME liver fellowship with a hybrid model of combined fellow and faculty time and two positions per year. In 2016 the Total Pancreatectomy with Islet Cell Autotransplant (TPIAT) program was started with the addition of Transplant Surgeon Marlon Levy, MD to the faculty. A total of 18 TPIATs were performed in 2022 for chronic pancreatitis, and they are one of the few centers offering this experimental therapy. Their cardiac program is the longest running on the east coast and the second oldest in the US. Over 680 heart transplants have been performed, and they offer an ACGME accredited Adult Cardiothoracic Anesthesiology fellowship with two fellows per year. There are no lung transplants being performed at present.
Many thanks to Dr. Liebman for sharing details of the transplantation program at VCU. If interested in having your program highlighted in the future, please contact David Rosenfeld, Mayo Clinic Arizona at Rosenfeld.david@mayo.edu
*The original newsletter identified VCU as performing the first identical twin kidney transplant in 1957. This was in error, the first kidney transplant was performed in an identical twin by Dr Joseph E.Murray in Boston in 1954. Correction made above.
Report from the Executive Council
By Susan Mandell, MD
We look forward to seeing SATA members at the in person SATA National Meeting, held at the IARS on April 17th, 2023, in Denver Colorado. Please remember to renew your membership for free entry to the meeting. SATA is pleased to announce it will hold the first combined meeting with the International Liver Transplant Society-SATA meeting just prior to the ASA in San Francisco. This has been a very popular meeting and well attended.
The Council is pleased to announce that there are now seven regional SATA meetings. Please check for the meeting closest to you. Service on the SATA Accessibility and Diversity Committee is now open to all members. The Vanguard committee has been revitalized and membership is open to all faculty who are within 5 years of residency completion or are younger than 42, please reach out to the SATA Office for more information.
Announcements
We are pleased to announce that SATA will be represented at the 10th Annual Korean Society of Transplant Anesthesiologists (KSTA) meeting in Seoul, Korea. During the Joint KSTA-SATA session (March 18, 2023 11:20-12:50 KST), moderated by Dr. Tetsuro Sakai and Justin Sangwook Ko, Dr. Satish Kumar will present on emerging evidence for coronary artery disease screening in liver transplant candidates and Dr. Ramona Nicolau-Raducu will present on post-reperfusion hyperfibrinolysis.
SATA is delighted to endorse the first International Symposium for Abdominal Organ Transplant (ISAOT) in Santiago, Chile, June 8-9, 2023.
This opportunity is presented by Dr. Klaus Torp at Mayo Clinic-Jacksonville (Founding member of SATA) who has supported the physician exchange program with the Clinica Alemanha in Santiago de Chile. Dr. Lucile Gignon (Faculty Anesthesiologist at the Clinica Alemanha in Santiago de Chile) is the local organizer of the meeting.
Attention liver transplant anesthesiologists and program directors! SATA is offering free 6 month membership to fellows! Please sign up by emailing sata@pacainc.com. We look forward to welcoming new fellow members!
Join the Vanguard Committee ***
Transplant Anesthesia Upcoming Meetings
SATA Meetings
SATA Tristate Regional Meeting – in person and virtual
March 25th, 2023, New York, NY
April 17th, 2023, Denver, CO
Other Meetings:
The 10th annual scientific meeting of the Korean Society of Transplantation Anesthesiologists (KSTA), March 18th, Seoul, Korea – in person and hybrid
Joint KSTA-SATA Session: 11:20 – 12:50 KST
IARS/AUA/SOCCA Annual Meeting – in person and hybrid
April 13-16th, 2023, Denver, CO
The 2023 International Congress of ILTS, ELITA and LICAGE
May 3-6, 2023; Rotterdam, Netherlands
American Transplant Congress (ATC) 2023 Annual Meeting
June 3-7, 2023, San Diego, CA
International Symposium for Abdominal Organ Transplant (ISAOT)
June 8-9, 2023, Santiago, Chile